Medical Billing for Denver Behavioral Health Practices
Behavioral and mental health services are growing faster than ever in Denver and across Colorado. But for most therapy and counseling practices, billing remains one of the toughest challenges from coding and compliance to claim submission and reimbursement delays.
If your clinic struggles with insurance denials, inconsistent cash flow, or compliance risks, this guide is for you. We’ll walk you through the essentials of behavioral health billing in Denver, explain how to maintain compliance, and share proven revenue cycle management (RCM) strategies to help your practice thrive in 2025.
Why Behavioral Health Billing Is So Complex
Behavioral health billing isn’t like general medical billing. It involves,
Longer therapy sessions with unique CPT codes (90832, 90837, 90846, etc.)
Frequent teletherapy claims and insurance parity rules
Coordination of care between psychiatrists, psychologists, and therapists
Strict HIPAA and payer specific documentation requirements

These complexities often lead to.
1. Claim denials due to incorrect time based codes
2. Payment delays because of parity law misunderstandings
3. Compliance risks with patient privacy
To avoid these pitfalls, behavioral health clinics in Denver are increasingly partnering with professional billing companies specializing in mental health billing across Colorado.
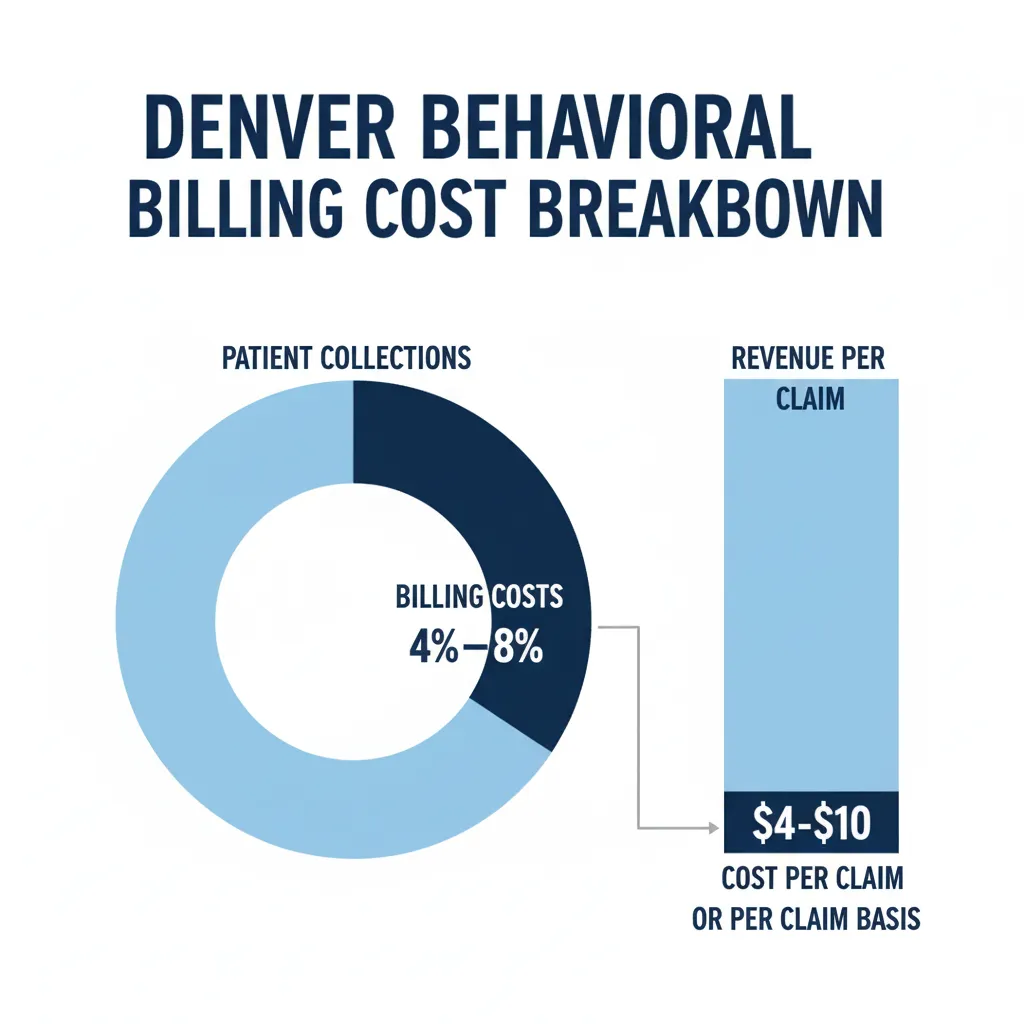
The Average Cost of Behavioral Health Billing in Denver
Most behavioral health practices in Denver pay.
4% to 8% of monthly collections, or
$4 to $10 per claim, depending on complexity and claim volume.
For group practices or counseling centers handling both in person and teletherapy sessions, hybrid pricing (mix of flat fee and percentage) offers flexibility and predictable budgeting.
Common Billing Challenges in Mental Health & Therapy Practices
1. Time Based CPT Codes Confusion
Each therapy session has specific duration based codes using the wrong one causes denials.
2. Telehealth Billing Barriers
Since 2020, teletherapy billing has grown exponentially, but payer rules differ widely. Some insurers require location modifiers or separate telehealth codes.
3. Prior Authorization & Credentialing
Many Denver practices face delays because insurance networks require prior authorization or incomplete credentialing data.
4. High Claim Denial Rate
Behavioral health has one of the highest claim denial rates in healthcare around 15% to 20% without proper billing oversight.
5. Privacy & Compliance Risks
HIPAA and HITECH compliance are critical for therapy notes, electronic records, and claims data. Any small error can lead to penalties.
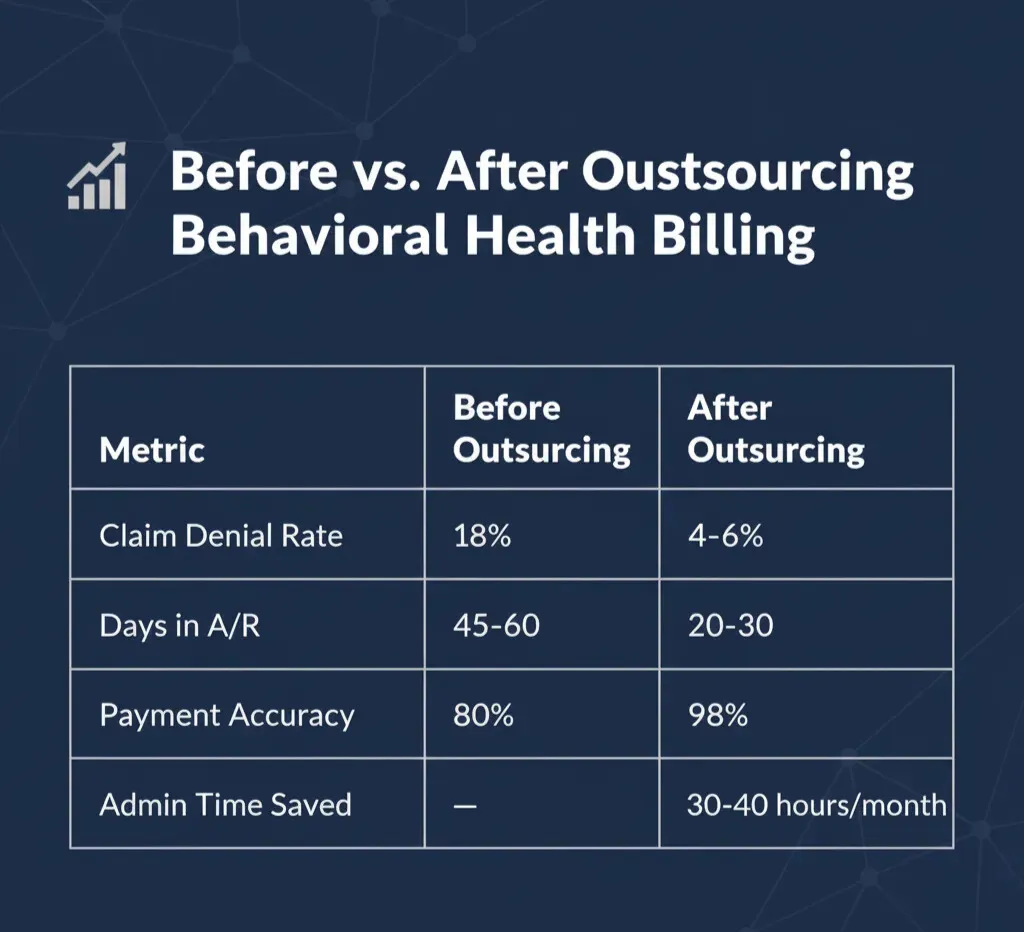
How Professional Behavioral Health Billing Improves Revenue
Outsourcing behavioral health billing in Denver delivers measurable results:
Revenue Optimization Tips for Denver Behavioral Health Practices
Verify Insurance Before Every Session
Prevent denials by confirming coverage and co-pays upfront.Use Correct Modifiers
Add telehealth modifiers (95 or GT) as per insurer guidelines.Automate Claim Tracking
Use automated billing tools to monitor every submission.Outsource Denial Management
Reduce rework time with professional RCM assistance.Schedule Monthly Revenue Reviews
Analyze claim trends and payment cycles for better forecasting.
Behavioral Health Billing Software Used in Denver
Popular systems among mental health providers include:
TheraNest
SimplePractice
Kareo
DrChrono
TherapyNotes
Ensure your billing partner integrates smoothly with these EMRs for seamless data exchange and reporting.
Real Client Case Study Denver Therapy Practice
A local Denver therapy center struggled with:
18% claim denials
50 day payment cycle
No telehealth reimbursement
After partnering with CureBill, they achieved:
92% first pass claim acceptance
30% faster reimbursements
Seamless telehealth billing compliance
Final Thoughts Billing Smart for Better Patient Focus
In the evolving healthcare landscape, mental health practices need more than just billing they need strategic RCM management that balances compliance, automation, and compassion.
By outsourcing to a trusted partner like CureBill, you can:
1. Simplify claim management
2. Maintain compliance
3. Improve revenue predictability
4. Focus more on patient well being
Visit CureBill’s HIPAA Compliant Billing Page or Schedule a Free Review today.
The cost of behavioral health billing services in Denver typically ranges from 4% to 8% of total collections or around $4 to $10 per claim, depending on the size of your mental health practice and claim volume. Outsourcing to a trusted company like CureBill ensures transparent pricing and maximum reimbursement for your therapy or psychiatry clinic.
Behavioral health billing is more complex because it involves time-based CPT codes, frequent session limits, and strict mental health parity and privacy regulations. Unlike general medical billing, therapy billing requires accurate documentation and modifier use to avoid denials — which is why many mental health providers in Colorado prefer outsourcing to experts like CureBill.
Yes, reputable behavioral health billing companies in Colorado, such as CureBill, are fully HIPAA and HITECH compliant. They use secure billing software and encrypted data systems to protect sensitive patient information while ensuring claim accuracy and compliance with federal regulations.
To reduce claim denials in your mental or behavioral health practice, make sure to verify insurance eligibility before each session, use accurate CPT codes and modifiers, and submit claims on time. Partnering with a specialized behavioral health billing company in Denver like CureBill can help automate denial management and improve claim acceptance rates.
Yes, teletherapy and telehealth sessions in Colorado are reimbursed at the same rate as in-person visits under mental health parity laws. CureBill’s behavioral health billing experts help ensure your telehealth claims are properly coded and paid on time, avoiding unnecessary delays or denials.
Top-rated mental health billing software for Colorado clinics includes TherapyNotes, SimplePractice, and TheraNest. These platforms integrate scheduling, documentation, and billing to streamline revenue cycles. CureBill can integrate with these systems or manage your billing directly to ensure smooth claims processing and reporting.
Absolutely! CureBill offers complete credentialing and payer enrollment services for therapists, psychologists, and behavioral health clinics across Colorado. From Medicare and Medicaid enrollment to private insurance panels, CureBill helps you get credentialed faster and start receiving payments without administrative stress.