What Is the Meaning of Billing Services in Healthcare?
Understanding billing services in healthcare is crucial for any medical practice, clinic, or hospital aiming to maintain a healthy revenue cycle. From processing insurance claims to managing patient invoices, healthcare billing plays a key role in ensuring providers get paid accurately and efficiently.
In this blog, we’ll explore what billing services in healthcare really mean, how they work, and why they are essential for healthcare providers of all sizes.
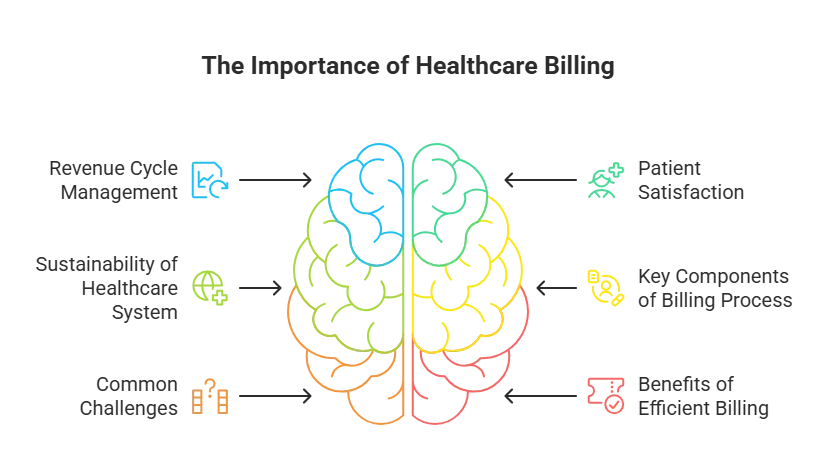
Why Healthcare Billing Matters
Medical billing is the process of translating healthcare services into billing claims. These claims are then submitted to insurance companies or patients to receive payment for services rendered.
It’s more than just paperwork billing services ensure.!
Timely reimbursements
Accurate coding
Reduced claim denials
Legal and compliance alignment
What Is Billing?
In simple terms, billing refers to generating invoices for services provided. In healthcare, this includes doctor visits, diagnostic tests, surgeries, and follow ups. Billing is done using standardized codes like CPT and ICD-10, essential for accurate documentation and reimbursement.
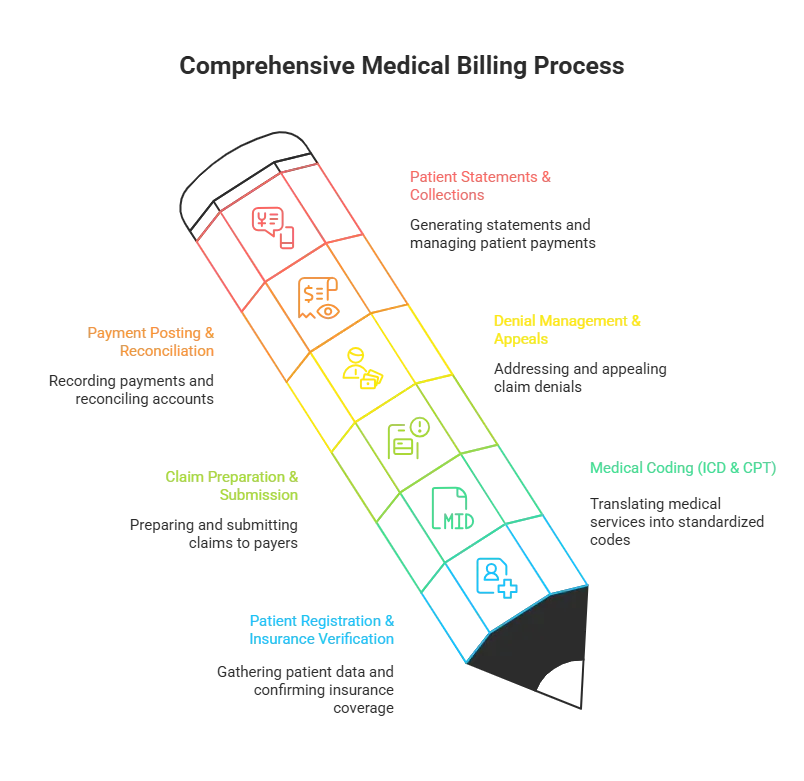
Key Components of Medical Billing Services
Medical billing isn’t just about sending invoices. It’s a structured workflow that includes several stages.
Patient Registration & Insurance Verification
The billing process starts with collecting patient demographics and verifying insurance coverage. This step ensures eligibility and reduces future rejections.
Medical Coding (ICD & CPT)
Certified coders translate diagnoses and procedures into medical codes. These codes are the language insurance companies understand.
Claim Preparation & Submission
Once coded, claims are prepared and submitted to the payer whether that’s private insurance, Medicare, or Medicaid.
Denial Management & Appeals
If a claim is denied or rejected, billing experts investigate the reason, make corrections, and resubmit.
Payment Posting & Reconciliation
After a claim is accepted and paid, the amount is posted in the patient’s record. Payments are reconciled to ensure no amount is left untracked.
Patient Statements & Collections
Patients may owe a balance after insurance. Statements are sent, and payments are collected with clear, itemized explanations.
Hospital Billing vs Outsourced Medical Billing Services
Hospital billing is often done in house, but many small clinics or independent practitioners opt for outsourced medical billing services.
Why Outsource?
Reduces administrative burden
Enhances billing accuracy
Speeds up revenue cycle
Offers scalability for growing practices
Medical billing services for small practices often include end to end solutions from coding to claim tracking, giving providers more time to focus on patient care.
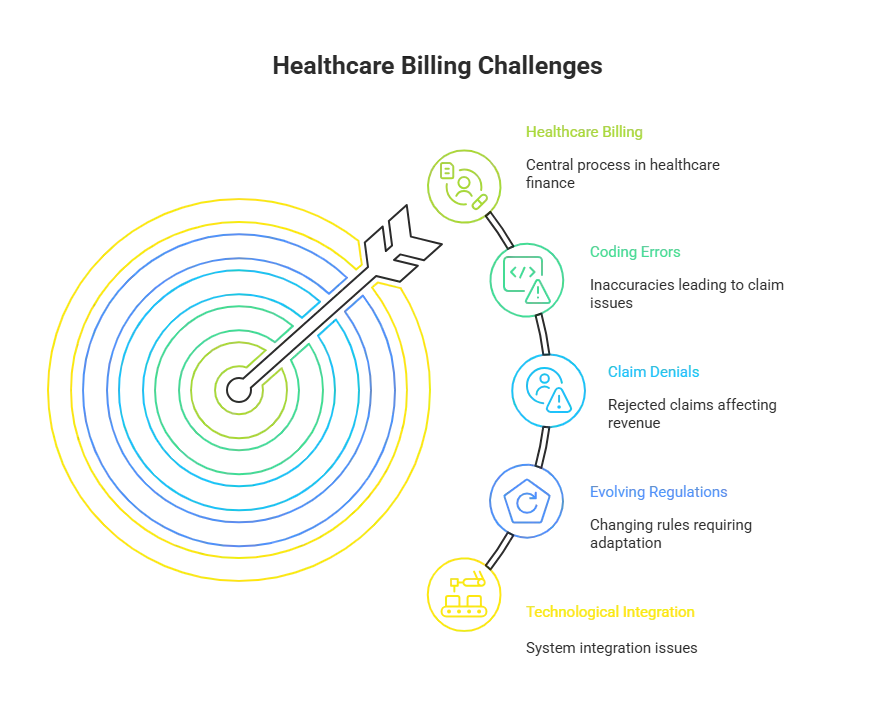
Common Challenges in Healthcare Billing
Claim Denials
Incorrect coding, missing documents, and eligibility issues cause thousands of rejections.
Delayed Payments
Without timely submission and follow up, practices face cash flow gaps.
Compliance Issues
HIPAA regulations require careful handling of sensitive information and claim documentation.
CureBill’s Solution
We proactively handle claim tracking, automate submissions, and ensure documentation compliance, helping you stay audit ready.
How CureBill Helps with Billing Services in Healthcare
At CureBill, we specialize in outsourced medical billing services tailored for.
Clinics
Hospitals
Solo healthcare providers
Specialty practices
What We Offer
Complete Revenue Cycle Management (RCM)
ICD-10 and CPT coding support
Claim submission and follow up
Denial appeals and analytics
AR Recovery & collections
Whether you’re searching for medical billing services near me or need help improving cash flow, CureBill offers secure, transparent, and efficient services.