Lab & Imaging Billing in Colorado How to Handle Denials from UnitedHealthcare & Anthem
Explain how diagnostic and imaging centers across Colorado from Denver to Colorado Springs face constant reimbursement challenges. Mention shrinking insurance payouts and frequent denials from major payers like UnitedHealthcare and Anthem. Introduce how professional RCM and denial management can save labs time and revenue.
Why Lab & Imaging Billing Is Getting Harder in Colorado
Shrinking Reimbursements
Insurance companies are tightening payment structures, reducing margins for diagnostic centers.
Complex CPT & Modifier Requirements
Each test or scan requires precise coding even a single missed modifier can trigger a denial.
Frequent Policy Updates from UnitedHealthcare & Anthem
Both payers regularly update prior authorization rules and billing codes, leading to unintentional claim errors.
Common Denial Reasons for Colorado Labs & Imaging Centers
Missing or incorrect CPT modifiers
Non-covered lab tests
Authorization not on file
Mismatched NPI or facility details
Claim submitted after filing limit
Pro Tip: Use denial analytics tools or outsource to an RCM partner to track and resolve repetitive issues faster.
UnitedHealthcare & Anthem Denial Patterns Explained
UnitedHealthcare Denials
Frequent rejections for lack of medical necessity documentation.
Commonly affects high-cost tests (toxicology, molecular, genetic).
Labs must submit physician order + supporting diagnosis codes.
Anthem Denials
Often deny due to authorization errors or invalid CPT crosswalks.
Anthem’s EDI system flags mismatched provider types and incorrect service locations.
How to Prevent These Denials
Keep payer bulletins updated.
Validate test codes before submission.
Automate pre-authorization workflows using billing software or outsource the process.
How Professional Billing Partners Help Colorado Labs Save Revenue
Real Time Eligibility Verification
Avoid denials by confirming coverage before performing tests.
Clean Claim Submission
Professional teams ensure CPT, HCPCS, and ICD-10 codes match payer policies.
Advanced Denial Management
Use analytics to categorize and appeal denials particularly from UnitedHealthcare and Anthem.
Revenue Recovery for Colorado Labs
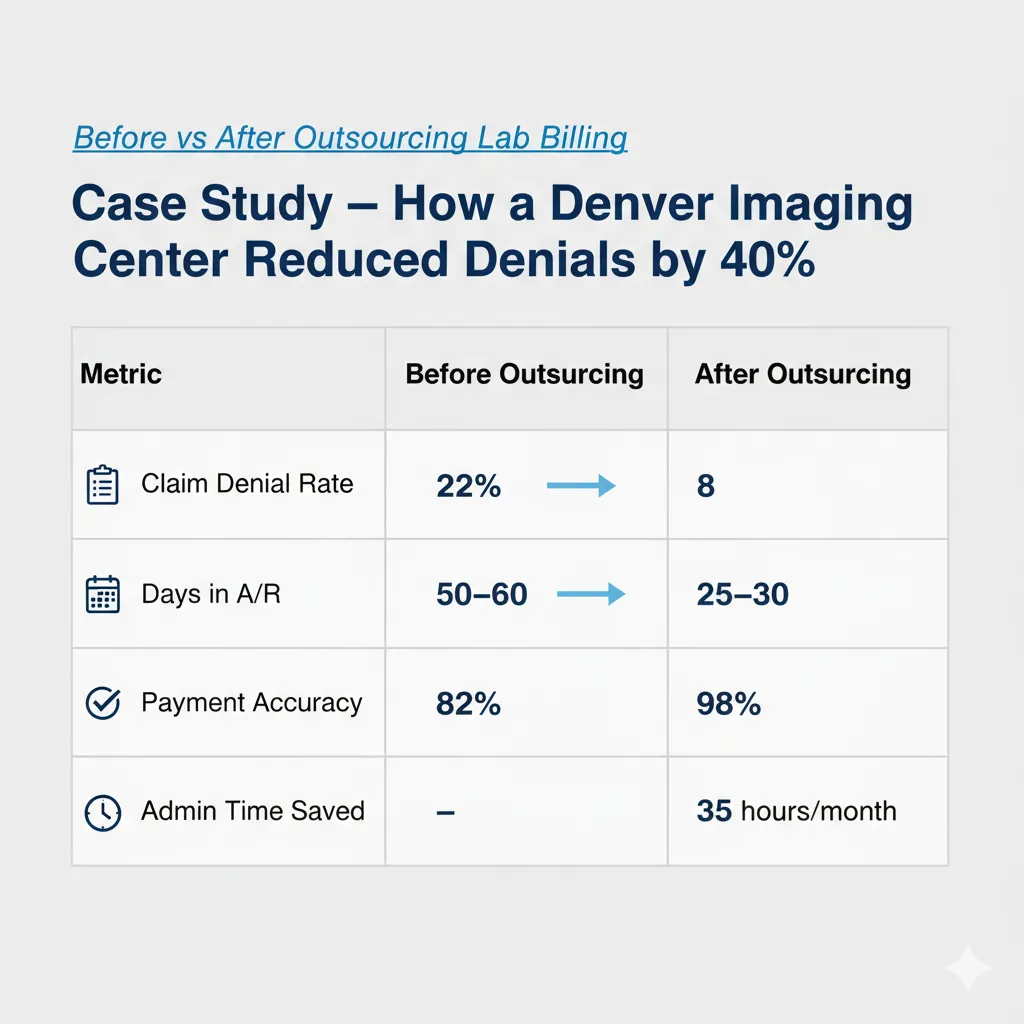
Outsourcing can increase collection rates by 20 to 30% and reduce A/R days by up to 50%.
Case Study How a Denver Imaging Center Reduced Denials by 40%
Best Practices for Lab & Imaging Billing in Colorado
1. Stay Updated with Payer Bulletins
Subscribe to payer updates from UnitedHealthcare and Anthem.
2. Use Specialty Billing Software
Systems like Kareo, AdvancedMD, and CollaborateMD are ideal for diagnostic billing.
3. Partner with a Colorado Based Billing Company
Local experts understand state regulations, CPT updates, and payer trends.
Why CureBill Is the Best Choice for Lab Billing in Colorado
CureBill provides complete lab billing services, including.
Denial tracking & recovery
Payer credentialing
Eligibility verification
Reimbursement optimization
Compliance with HIPAA & payer rules
Whether you run a diagnostic center in Colorado Springs or an imaging lab in Denver, CureBill ensures smoother claim submission, faster payments, and fewer denials
Final Thoughts
In a state where payer scrutiny is rising, efficient billing can make or break profitability. Partnering with experts helps labs not only recover revenue but also stay compliant and scalable.
In Colorado, most lab billing denials occur due to missing modifiers, outdated or invalid CPT codes, and lack of prior authorization—especially with major insurers like UnitedHealthcare and Anthem. Ensuring proper documentation and payer compliance can significantly reduce denials.
Denver imaging centers can lower claim rejections by verifying patient eligibility before every test, using up-to-date CPT and ICD-10 codes, and outsourcing to specialized imaging billing services in Denver that understand payer-specific rules and compliance.
Top-rated lab billing software in Colorado includes AdvancedMD, Kareo, and CollaborateMD. These systems help automate claims, track denials, and integrate with EMRs for faster payments and better reporting accuracy.
With professional outsourced medical billing in Colorado, payments typically arrive within 20–30 days, compared to 45–60 days for in-house teams. Outsourcing improves cash flow and reduces administrative delays.
Yes, leading companies like CureBill offer HIPAA and HITECH-compliant billing services, ensuring full data security and patient confidentiality for labs, imaging centers, and diagnostic facilities across Colorado.
Absolutely. CureBill’s denial management experts specialize in recovering rejected claims from payers like UnitedHealthcare and Anthem. Their proactive tracking and appeal system help maximize collections and minimize revenue leakage.
On average, lab billing services in Colorado cost between 4%–7% of total monthly collections, depending on claim complexity, volume, and specialty. This makes outsourcing a cost-effective solution compared to hiring in-house billing staff.